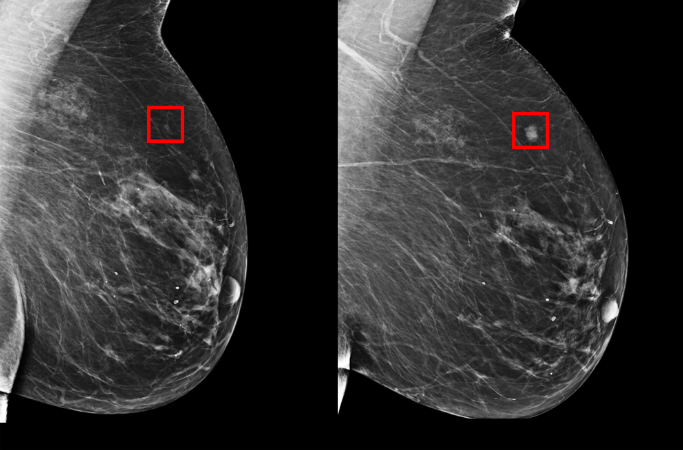
Our imaging technology has advanced significantly in the past decade but even so, the vast majority of breast cancer patients often do not manage to catch the illness in its incipient stage and for others, by the time it is diagnosed, it is already too late.
Whenever breast cancer, or any other type of cancer, is diagnosed in its later stages, it means that the treatments needed are very aggressive and the chances of recovery minimal.
Identifying patients at risk before the disease starts to develop is crucial and now, an MIT team from the Computer Science and Artificial Intelligence Laboratory (CSAIL), in collaboration with the Massachusetts General Hospital (MGH) have created a deep learning model that is capable of using a mammogram to predict if a patient has a chance of developing breast cancer in the future.
The model was trained on the mammograms and known outcomes of over 90,000 patients that have been treated at the MGH and has picked up on the subtle patterns that can indicate a predisposition towards the illness.
“Since the 1960s, radiologists have noticed women have unique and widely variable patterns of breast tissue visible on the mammogram.” Constance Lehman, professor of radiology at Harvard Medical School and Division Chief of Breast Imaging at Mass General Hospital said “These patterns can represent the influence of genetics, hormones, pregnancy, lactation, diet, weight loss and weight gain. We can now leverage this detailed information to be more precise in our risk assessment at the individual woman level.”
There is more good news: the AI model works exactly the same on both black and white patients. There has been a disparity between black and white women when detecting breast cancer, as most of the breast cancer guidelines are based on white populations.
Now, thanks to this AI, that will no longer be the case because the team trained their AI on data that included an equal amount from both populations.
“It’s particularly striking that the model performs equally as well for black and white people, which has not been the case with prior risk assessment tools” Dr. Allison Kuarian, Associate Professor of Medicine and Health Research and Policy at Stanford University to MIT said “If validated and made available for widespread use, this could really improve on our current strategies to estimate risk.”
Mammography reduces breast cancer through randomized clinical trials but the debate on how often to perform the screenings and when to start them is still ongoing – the American Cancer Society recommends an annual screening after age 45, while in the UK women aged 50 to 71 are invited to a screening only every 3 years.
“Rather than taking a one-size fits all approach, we can personalize screening around a woman’s risk of developing cancer,” MIT Professor Regina Barzilay, a breast cancer survivor herself, has said “For example, a doctor might recommend supplemental MRI screening for women with high model-assessed risk.”
The MIT AI managed to predict risk at a better rate than any of the other previous approaches and placed 31% of cancer patients in its high-risk category, when compared with only 18% for the other, traditional methods.
Adam Yala, PhD student at MIT CSAIL and co-author of the study has said that their goes “is to make these advancements a part of the standard of care. By predicting who will develop cancer in the future, we can catch cancer before symptoms ever arise and hopefully save lives.”
Follow TechTheLead on Google News to get the news first.